Invented by Hakki Refai, Badia Koudsi, Optecks LLC
Medical 3D scanning and mapping systems use various technologies such as computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound to capture detailed images of the human body. These images are then processed and converted into 3D models, allowing healthcare professionals to visualize and analyze the patient’s anatomy in a more comprehensive manner.
One of the key drivers of the market growth is the increasing demand for personalized medicine. With the advancements in genomics and molecular biology, healthcare professionals are now able to tailor treatments to individual patients based on their genetic makeup. Medical 3D scanning and mapping systems play a crucial role in this process by providing detailed information about the patient’s anatomy, allowing for more precise treatment planning and delivery.
Another factor contributing to the market growth is the rising prevalence of chronic diseases such as cancer and cardiovascular diseases. These conditions often require complex surgical procedures, and medical 3D scanning and mapping systems help surgeons to accurately plan and execute these procedures. By providing detailed 3D images of the affected area, these systems enable surgeons to navigate through complex anatomical structures and minimize the risk of complications.
Furthermore, the increasing adoption of minimally invasive procedures is also driving the demand for medical 3D scanning and mapping systems. Minimally invasive procedures offer several advantages over traditional open surgeries, including shorter recovery times, reduced scarring, and lower risk of infection. Medical 3D scanning and mapping systems play a crucial role in these procedures by providing real-time guidance and visualization, allowing surgeons to perform complex interventions with precision and accuracy.
The market for medical 3D scanning and mapping systems is also benefiting from advancements in technology. The development of more compact and portable systems has made these technologies more accessible to healthcare facilities of all sizes. Additionally, the integration of artificial intelligence and machine learning algorithms has further enhanced the capabilities of these systems, allowing for automated analysis and interpretation of the captured images.
However, despite the numerous benefits and growth opportunities, there are still some challenges that the market faces. One of the major challenges is the high cost associated with these systems. The advanced technologies and complex algorithms used in medical 3D scanning and mapping systems make them expensive to develop and maintain. This cost is often passed on to the end-users, limiting the adoption of these technologies in resource-constrained healthcare settings.
Moreover, the regulatory landscape surrounding medical 3D scanning and mapping systems is still evolving. As these technologies become more advanced and sophisticated, regulatory bodies are working to establish guidelines and standards to ensure their safe and effective use. This regulatory uncertainty can slow down the market growth and hinder the adoption of these technologies.
In conclusion, the market for medical 3D scanning and mapping systems is witnessing significant growth due to the increasing demand for personalized medicine, rising prevalence of chronic diseases, and the adoption of minimally invasive procedures. However, challenges such as high costs and regulatory uncertainties need to be addressed to fully unlock the potential of these technologies. As technology continues to advance and costs decrease, medical 3D scanning and mapping systems are expected to become an integral part of healthcare delivery, improving patient outcomes and revolutionizing the field of medicine.
The Optecks LLC invention works as follows
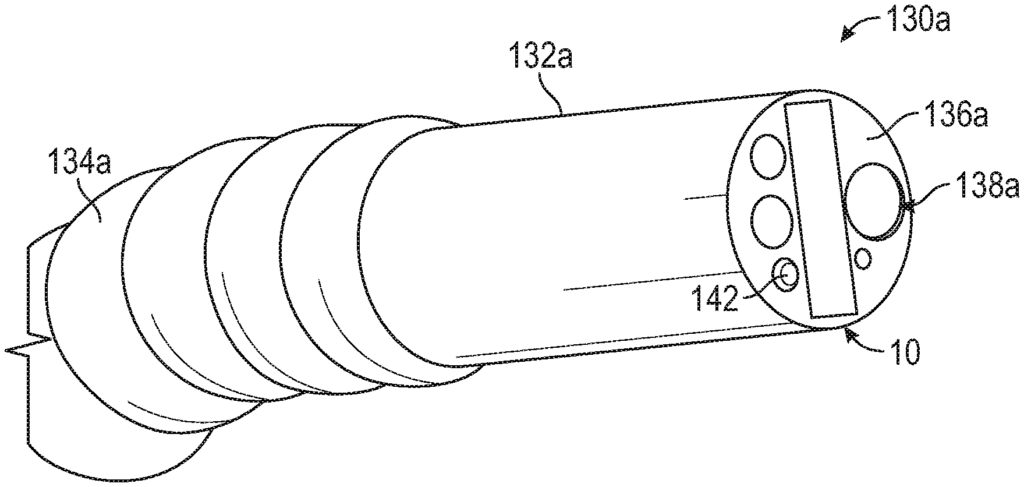
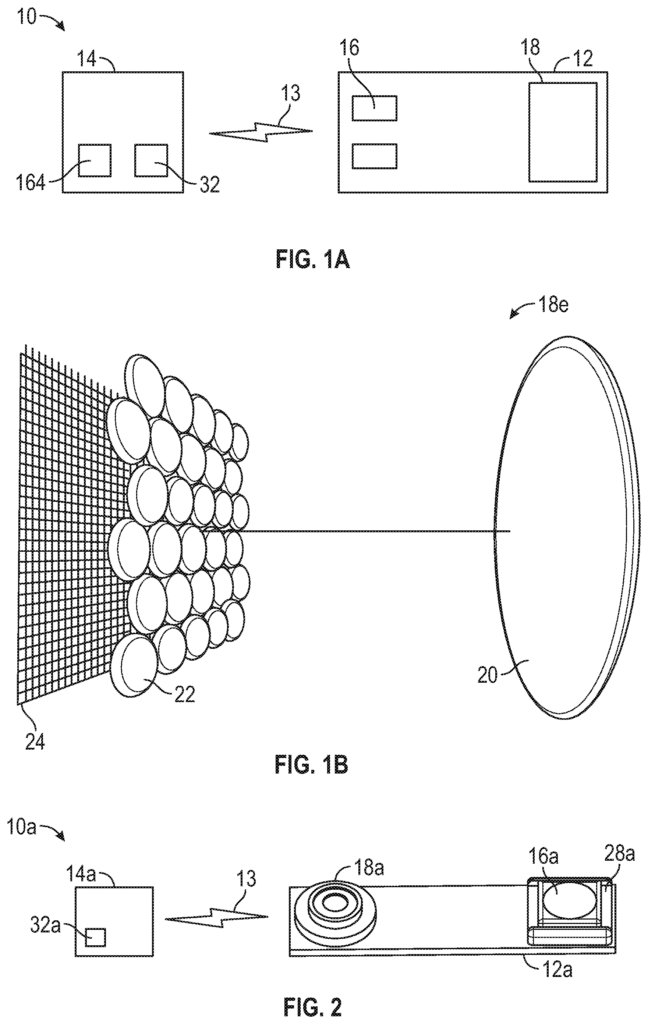
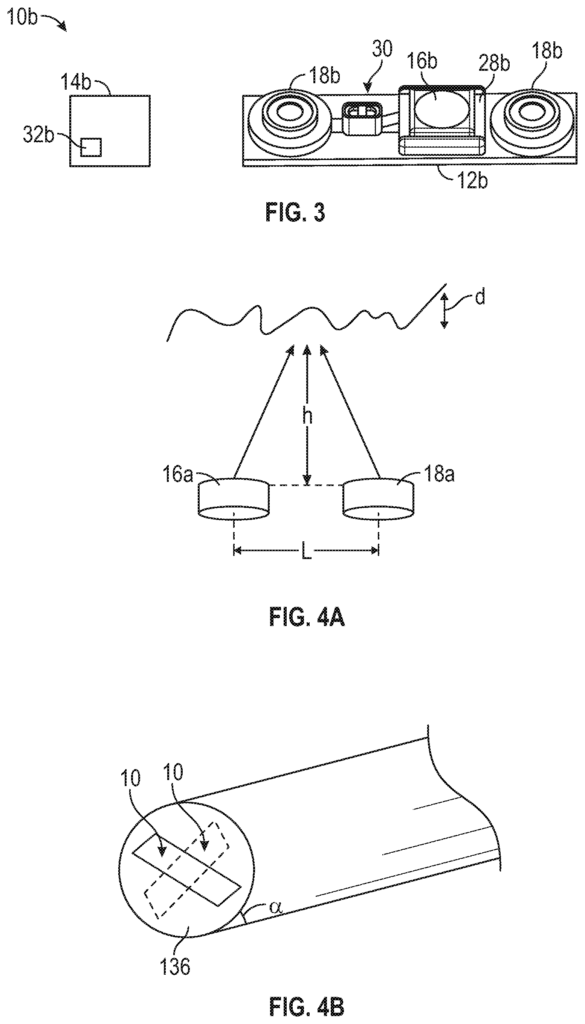
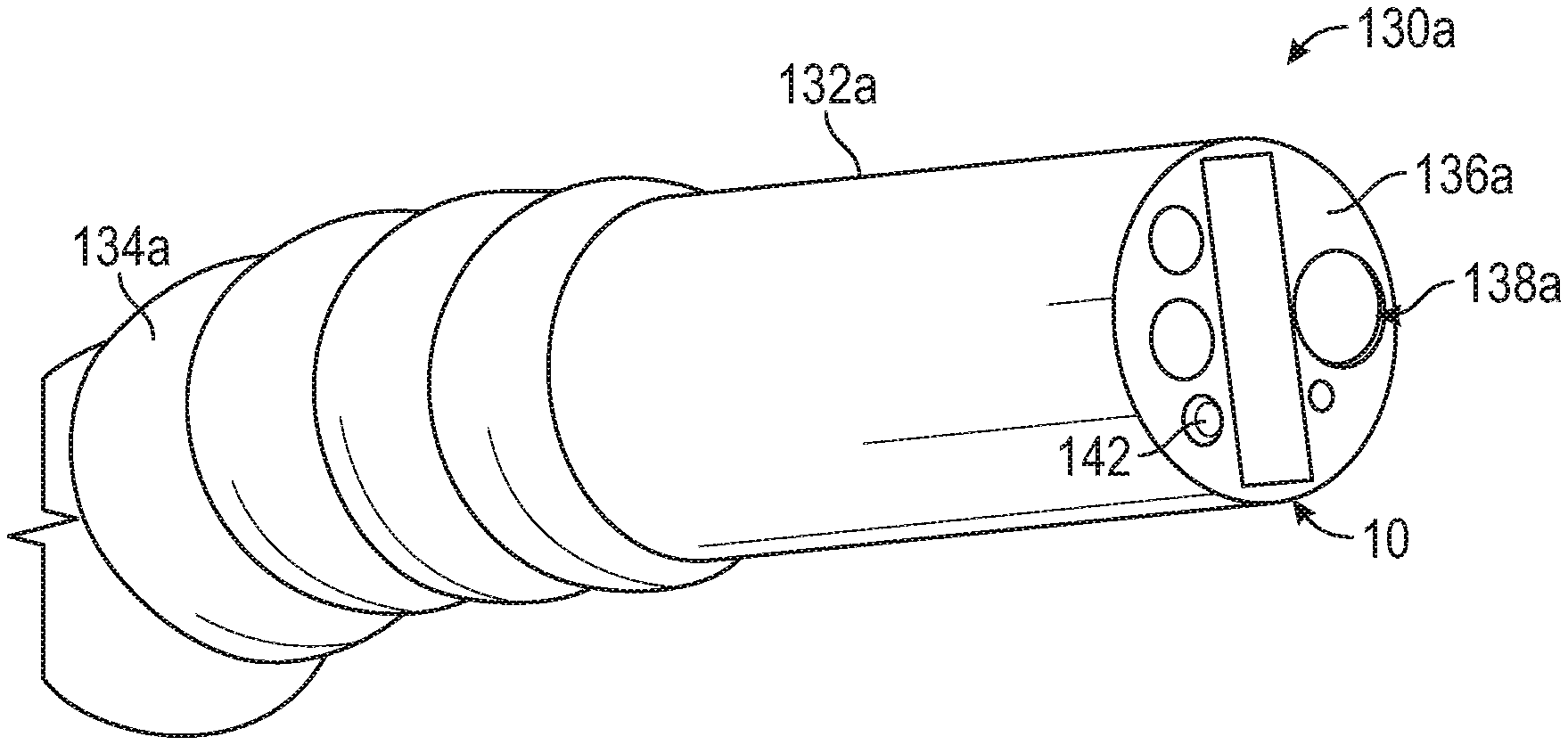
Systems and Methods for Three-dimensional Imaging, Modeling, Mapping, and/or Control Capabilities in Compact Size, suitable for Integration with or Augmentation of Robotic, Laparoscopic, and Endoscopic Surgical Systems.” The systems include at least an optical source configured to cast a projection onto a surgical environment or endoscopic area, and at lease one camera positioned in order to capture at leat one image from the surgical environment or endoscopic area.
Background for Medical 3D (3D) Scanning and Mapping System
Surgeons performed over 7.5 millions laparoscopic surgeries worldwide last year, including over 3.5 Million laparoscopic surgeries in the United States alone. By 2021, the U.S. is expected to perform 4 million laparoscopic surgeries due to new innovative devices that are expected to improve laparoscopic results and make them more efficient. The limited range and availability of laparoscopic and robot assisted surgical tools will continue to limit the growth of these techniques. This is in contrast to open surgery, where surgeons can use a wide variety of tools during the procedure. Even with these limitations, laparoscopic surgeries, robotic surgery advances introduced by Intuitive Surgical with the daVinci System, and planned robotic surgical systems introductions from other manufacturers continue to expand the use of such systems. For example, there are over 4,271 daVinci Systems deployed and in operation worldwide.
Colonoscopy is a vital tool for detecting colorectal carcinoma, which is the second-leading cause of cancer-related death in the U.S. with one in three patients dying from it. Correctly performed colonoscopies are able to detect precancerous polyps, adenomas and facilitate the removal or treatment of these polyps, adenomas and early detection of colorectal carcinoma. The lack of trained professionals and a missed rate of 20.7% for polyps, and 22.9% respectively, by professionals who are trained, limits the number of patients who undergo the procedure. The need for colonoscopy will increase as the population grows older, even though the number of professionals trained to perform this procedure is not growing fast enough to meet the demand.
The prior art relies on visible light systems to provide images of surgical spaces or colonoscopies, but they lack the capabilities needed to improve the performance of minimally invasive surgery and colonoscopy. The visible light systems are unable to provide accurate intra-operative measurement. Prior to recent times, most measurement methods involved inserting a flexible ruler through the surgical sleeves or measuring the surgical instruments prior to surgery. Other subjective measurements were based on surgeons’ prior experience. In hernia surgery, failures to accurately measure size and shape can result in incorrect sizing and forming of patches [1,2], failing to place suture to close the hernia within 3 to 6 mm of fascial edges [4-7], or errors when preparing pockets to insert the patch. The second problem is that the current visible light systems can only look forward. This means the physician will miss the details on the side of the tool, unless they turn the instrument so it looks in the opposite direction. For example, during colonoscopy, the physician might miss small polyps or adenomas that have a color that blends with the colon tissue’s coloring, or are hidden behind folds. This prevents treatment until polyps become dangerous to the patient.
The current visible light systems are unable to provide 3D data, mapping and modeling of the procedure space. This limits the monitoring of the environment in surgical or colonoscopy operations, the ability of providing data to the doctor that could help guide the endoscope or surgical tools, and the capability to compile patient records for monitoring their health over time. During abdominal surgery, for example, the surgeon needs to avoid damaging vital organs or blood vessels, which could harm the patient. In order to achieve optimal colonoscopy results, the endoscope must be positioned at or near the center of colon. The cecal intubation should also take place within a time frame that is optimal. The visible light system is unable to provide enough data to develop autonomous or semi-autonomous robots that can perform difficult tasks like suturing, guiding endoscopes through curved spaces such as the colon, the brachial tubes and the throat. The visible light system cannot also produce detailed three-dimensional mapping, imaging, and modeling of the procedural area that would support augmented-reality-based displays for surgeons or colonoscopy users and support the creation of simulators to support surgical and colonoscopy procedure.
The US surgeons perform between 350,000 and 500,000 ventral hernia repair procedures each year, while about 30% of these are performed using minimally-invasive techniques [9-10]. According to the CDC, colonoscopies have prevented or treated 66,000 cases of colorectal carcinomas between 2003 and 2007 and saved more than 32,000 lives.
In many surgical procedures including hernia repair, surgeons must make precise incisions or cut to ensure a successful procedure. For example, a surgeon may need to make a precise cut to insert a medical instrument or access a surgical area safely. They might also have to make a precise cut to remove unwanted tissue and minimize trauma to healthy tissue around the tumor. In non-invasive procedures, surgeons are unable to use the same measurement tools as in open surgery procedures. Current non-invasive systems also provide very limited tools, if they even exist, for taking measurements during the procedure. Surgeons can only develop the skill to accurately measure distances within the operating space using the visible light system after extensive training and practice. CT scans are used by many medical facilities to determine the size of the patch before surgery. The mesh area-to-defect area (M/D), ratio is the only independent predictor of hernia recurrence. [1] Recurrence rates for M/D?8 range from 70% to 35%. Even though the CT scan is performed before surgery, the surgeon must often perform intraoperative measurements in order to increase the chances of success. If the hernia is irregularly shaped, for example, the surgeon will need to accurately measure the shape, circumference and total area of the hernia in order to ensure that the patch overlaps. To ensure the correct overlap, the surgeon must accurately measure pockets created intraoperatively for the mesh patch. The best outcomes are achieved by ensuring that the defects and pockets are measured accurately. In fact, 8.5% of all hernia cases recur because the patch was too small. The surgeon must place the stitches within 3-6mm of the fascial border [4-7] to close the hernia. This precision requires millimeter-accurate imaging. A system that can provide real-time proximity measurements is necessary to avoid damage or trauma of large blood vessels and critical organs.
In colonoscopy several factors can contribute to missed polyps or adenomas. These include the insertion and removal time, the cecal intubation rates, the quality of bowel prep, the size and shape of polyps as well as the number and number. The imaging system is also important, especially for detecting adenomas. The presence of an assistant to enhance the abilities of the physician performing colonoscopy, whether it is a primary physician or a physician who has not had training in this procedure, increases the effectiveness of the procedure. The assistant can be a person physically present during the procedure or a person who is on call to support difficult parts of the process. It could also include adding data, text, icons and highlighting to the visible light images based on high-accuracy, real-time mapping of colon tissue around endoscope. The system would combine high-accuracy scanner hardware with sophisticated mapping software to provide the assistance required to improve the success rate for colonoscopies.
Intuitive Surgical, after years of research and development, introduced a mechanical intraoperative measurement feature to the DaVinci robotic surgery system in early 2018. The system allows a surgeon to click a button and physically move the surgical head. They then click the same button. The software uses inputs from the head of the surgical instrument to measure distance. Operators must make multiple passes to measure in different directions. “The measurement system is not suitable for colonoscopy procedures.
Auris Surgical Robotics has recently introduced the Monarch Platform. This flexible robotic endoscopic device received FDA approval for bronchoscopic surgery. The Auris system creates a three dimensional map using a collection two-dimensional CT scans taken before surgery. The operator guides the endoscope using the three-dimensional maps [14-23]. The three-dimensional maps are not accurate enough to detect polyps or adenomas of any size, but especially those less than 6mm, making them unsuitable for colonoscopy. Sensors give additional feedback about the endoscope?s orientation and position.
Advantis Medical Systems has recently launched its Third Eye Panoramic System to help improve the detection of polyps or adenomas hidden behind folds on the colon wall. Advantis’ system is a module with two wide-angle source-camera pair mounted sideways on the endoscope. The operator can see the walls surrounding the endoscope and the illumination penetrates a greater fraction of folds with the additional imaging systems. The design of the system presents significant difficulties to the operator. The system displays on screen three separate images, one for each of the cameras, which requires the operator to monitor and process the three images simultaneously to detect polyps, instead of just one integrated view of colon.
BRIEF DESCRIPTION ABOUT THE VIEWS FROM THE DRAWINGS
For consistency, like reference numbers are used to refer to elements that are similar. To ensure clarity, not all components may be labeled on every drawing.
FIG. “FIG.
FIG. “FIG. 1 .
FIG. “FIG.
FIG. “FIG.
FIG. “FIG.
FIG. “FIG.
FIG. “FIG.
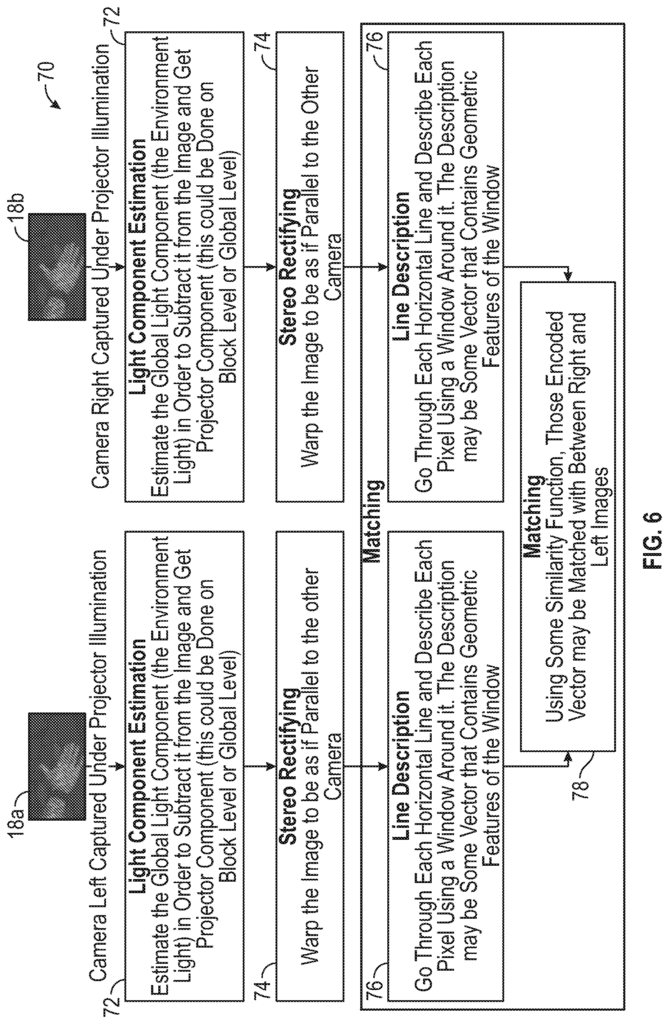
FIG. “FIG. 6 is a flowchart illustrating another set of operations and calculation performed by an imaging reconstruction system in order to produce three-dimensional models and/or measurements data according to the present disclosure.
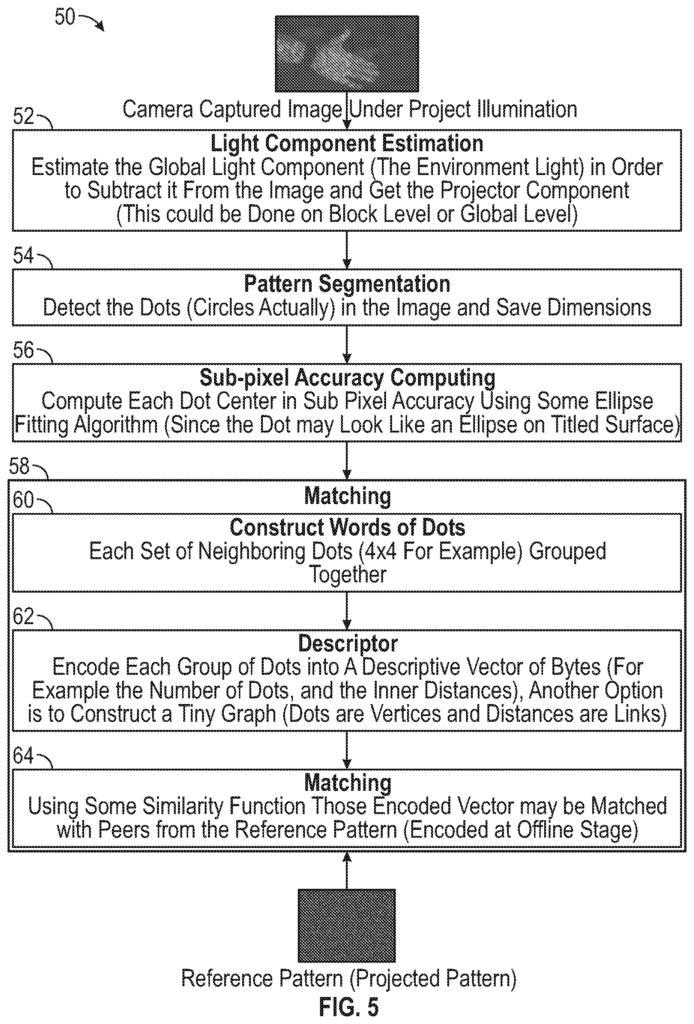
FIG. “FIG.
Click here to view the patent on Google Patents.
Leave a Reply