Invented by David M. Eddy, Joshua Adler, MacDonald Scott Morris, Azara Intermediate LLC, Mddatacor LLC
The market for health care quality measurement includes a variety of stakeholders, including government agencies, private companies, and non-profit organizations. These stakeholders are involved in developing and implementing quality measures, collecting and analyzing data, and reporting on the performance of health care providers.
One of the main drivers of the market for health care quality measurement is the shift towards value-based care. This model of care focuses on improving patient outcomes and reducing costs, and quality measurement is a key component of this approach. Providers are increasingly being incentivized to improve the quality of care they provide, and quality measures are being used to track their progress.
Another driver of the market for health care quality measurement is the increasing use of electronic health records (EHRs). EHRs provide a wealth of data that can be used to measure the quality of care provided to patients. This data can be used to identify areas for improvement and to track progress over time.
The market for health care quality measurement is also being driven by the increasing use of patient-reported outcomes (PROs). PROs are measures of the patient’s health status and quality of life, and they are being used to assess the effectiveness of treatments and interventions. PROs are also being used to measure the quality of care provided by health care providers.
The market for health care quality measurement is expected to continue to grow in the coming years. As the health care industry continues to shift towards value-based care, quality measurement will become even more important. Providers will need to demonstrate that they are providing high-quality care in order to compete in this new environment.
In conclusion, the market for health care quality measurement is a growing and important area of the health care industry. It is being driven by the shift towards value-based care, the increasing use of EHRs, and the use of PROs to measure the quality of care provided to patients. As the industry continues to evolve, quality measurement will become even more important in ensuring that patients receive the best possible care.
The Azara Intermediate LLC, Mddatacor LLC invention works as follows
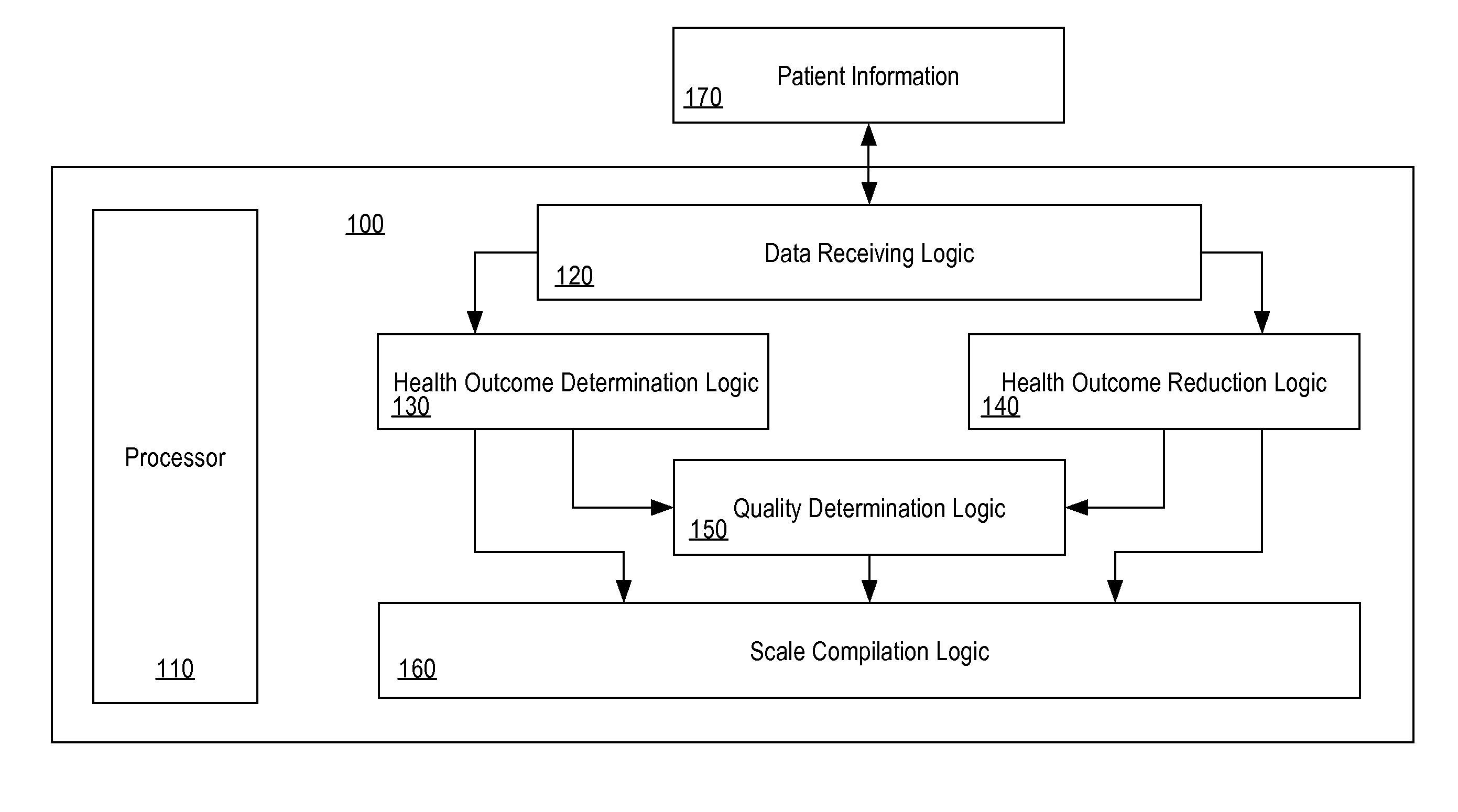
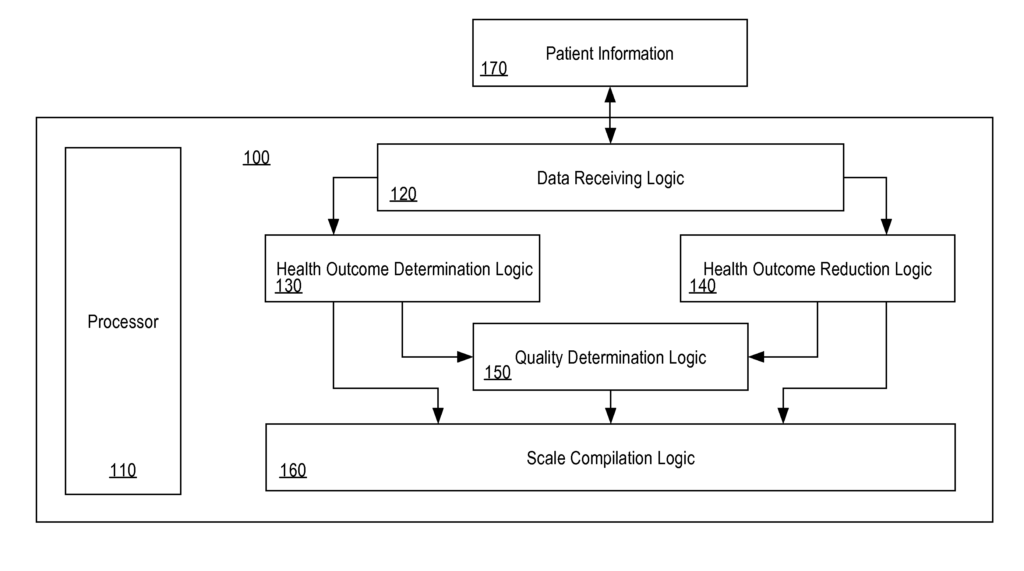
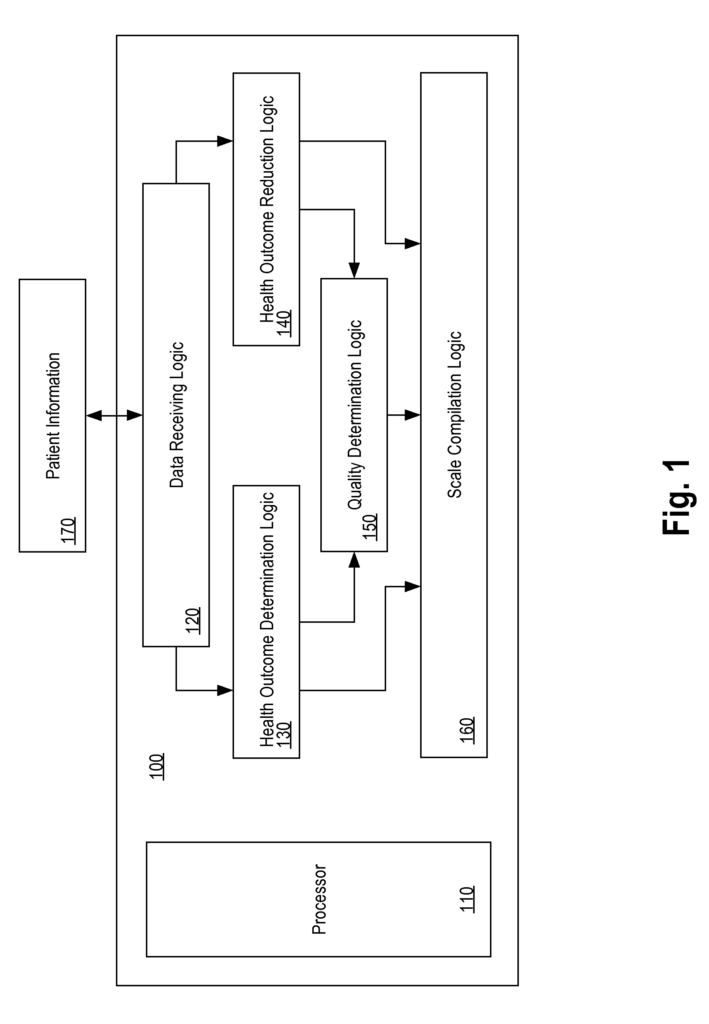
A method for determining the quality of healthcare provided by a provider of healthcare to individuals within a population” is disclosed. The disclosure relates to a data processing apparatus having one or more processors. A population of individuals is provided with data representing biomarkers. Risks at baseline and current are calculated. The risk reduction values are calculated. A quality score is calculated based on the current level of risk reduction. The quality score is then mapped onto a scale. The global quality score is a significant improvement over previous performance measures.
Background for Health care quality measurement
The introduction of performance measurement in healthcare came as a result of the wide variation in practice among doctors, ineffective care and high rates of patients not receiving treatments that professional organizations and guidelines had determined to be effective. Since the trend of performance measurement began, programs like the Healthcare Effectiveness Data and Information Set by the National Committee for Quality Assurance (NCQA), have encouraged an increase in the use evidence-based treatment. In the first 10 years of HEDIS, it is estimated that improvements in performance have prevented 1,900,000. heart attacks, 800,000. strokes and 100,000 cases end-stage kidney disease.
Performance measurement has a wider role than just measuring quality. Performance measurement is used increasingly in “pay for performance” programs. Incentives for healthcare professionals. These programs may allow physicians to earn bonuses based partially or completely on performance metrics.
Most methods for measuring performance are based upon guidelines. The HEDIS blood-pressure measure, for example, counts the number of people who have a diagnosis or hypertension and whose systolic (SBP), is less than 140. This measure is based on the JNC 7 guideline. Performance measures are based on the same evidence as guidelines like the JNC 7 guideline. It is easier to ensure that health outcomes will be improved by improving performance on these measures. Aligning performance measures with guidelines ensures that physicians receive consistent messages. They are not told to do one thing in a guideline and their performance is assessed against a completely different standard.
Guidelines focus on the actions that providers should take, and how to perform them. Measures based on treatment and process targets do not provide information on the health outcomes. They also don’t allow comparisons between different measures and they aren’t designed to encourage the search for the most efficient and effective ways to improve the outcomes.
Performance Measures based on Guidelines also have the effect that guidelines become rules. Providers are often penalized for not adhering to the measure even when it calls for an inappropriate or unnecessary action. They also get no credit if they go beyond the immediate goal of the measure. Performance measures that are based on specific guidelines can devalue other guidelines. If providers do not follow guidelines that have no performance measures, there is no penalty. However, if they achieve the goal of the measure then the provider has provided high-quality care and may stop providing care. There is also an incentive for providers to allocate resources in a way that prioritizes guidelines with performance measures and avoids those without.
Guidelines have been issued independently of each other, as they are developed by groups with the most expertise and interest. There is no way of comparing measures or determining their relative importance. Further, giving equal weight to each performance measure can lead to a misaligned priority. As an example, a part of the third recommendation of the Adult Treatment Panel III, referred here as ATP III, is the panel’s expert report on the detection, evaluation and treatment of high cholesterol in adults. Controlling LDL cholesterol below 100 mg/dL is recommended for people with cardiovascular disease. This reduces their 30-year risk of MI by 39%. ATP III recommends lowering LDL cholesterol below 160mg/dl in patients with fewer risk factors. This reduces their 30-year MI risk by approximately 5%. The two parts of ATP III have not only very different effects on the risk of the patient, but also very different costs. “Giving these two recommendations equal weight leads to an inefficient use and misplaced focus.
Most guidelines are clinically simple and focus on a single factor, like a patient’s pressure. Guidelines tend to use sharp cutoff points to distinguish between those who need to be treated and those who don’t. A hypertension guideline, for example, recommends that blood pressure should be kept below 140/90 mmHg. This simplifies guidelines for doctors and patients, but it can also harm quality and efficiency by encouraging the wrong treatment.
Current methods of measuring performance are not sufficient.
The approaches described herein are possible approaches, but not necessarily those that have been used before. It is not possible to assume that any of these approaches are prior art, except as otherwise stated.
The following description provides a detailed explanation of the invention. However, it will become apparent that the present invention can be used without these details. Other instances of well-known devices and structures are shown in block diagrams to avoid obscure the invention.
A method for determining the quality of healthcare provided by a provider of healthcare to individuals within a population has been disclosed.
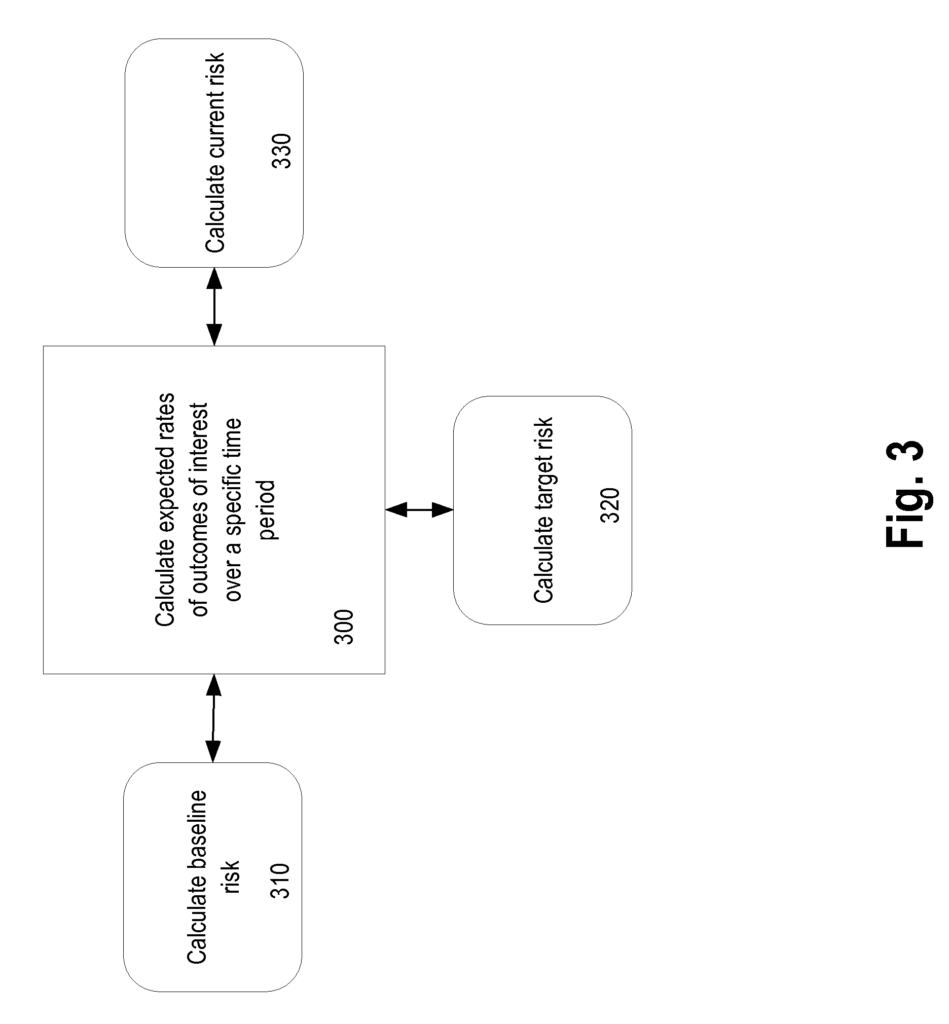
In one embodiment, data representing at least a part of a population’s individuals is received. Based on the baseline treatment data associated with the population, a baseline health outcome metric is calculated. Based on the current treatment data for a population, a current health outcome metric can be determined. The current health outcome value reduction is calculated as the difference between the baseline health outcomes metric and current health outcomes metric.
In one embodiment, the health outcome is a metric of quality of living that represents a value of quality of the life associated with one or more health outcomes. The baseline health outcome represents a population’s baseline quality of the life, and the present health outcome represents the population’s current quality of the life.
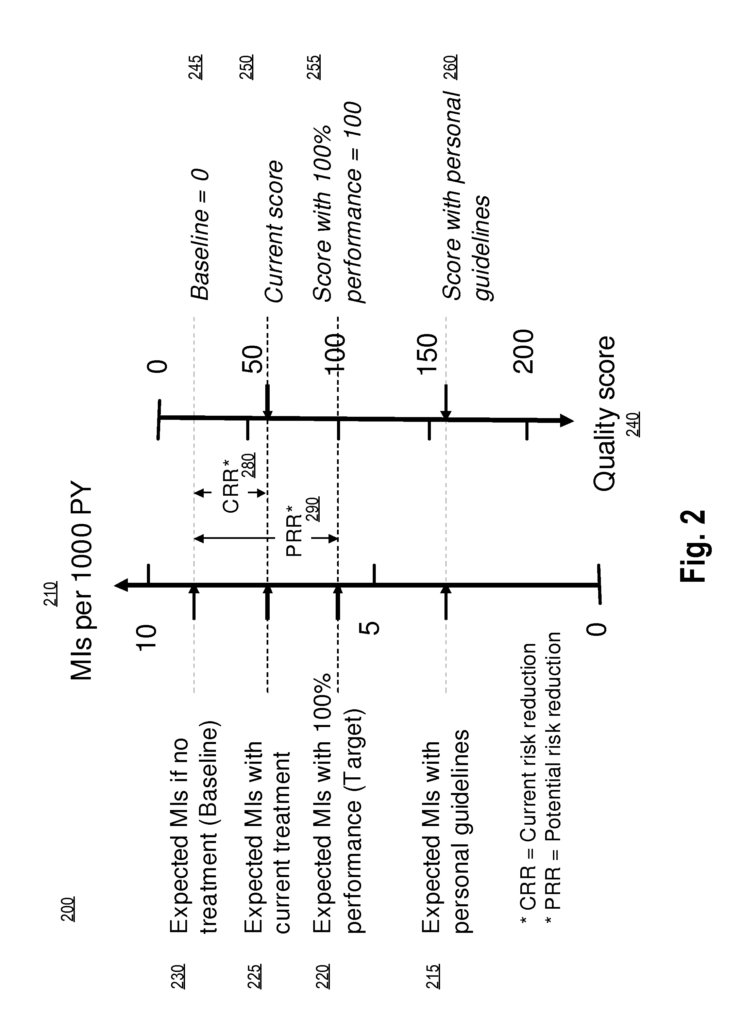
In one embodiment, a health outcome target metric that represents a desired level of quality of life for a population is determined. Also, a reduction potential in health outcome metrics as a result from the difference between baseline health outcomes and target health outcomes are also determined. The potential health outcome value is at least partially used to determine the quality score. The quality of care scale is assigned the target health outcome metric.
In one embodiment, the health outcome metrics are risk metrics that represent the risk for the population to incur the one of more healthcare outcome. The baseline health outcome measures the risk the population will incur one of more healthcare outcome. And the current health outcomes measure the present risk the population has of incurring these healthcare outcomes.
In one embodiment, the potential reduction in health outcome metrics is determined by comparing the baseline health outcomes metric with the target health outcomes metric. A quality score based, at least in part, on the target health outcomes metric and the potential health outcome metrics is assigned to the scale of quality care. In one embodiment, determining the quality score value includes dividing the current outcome metric by potential outcome metric.
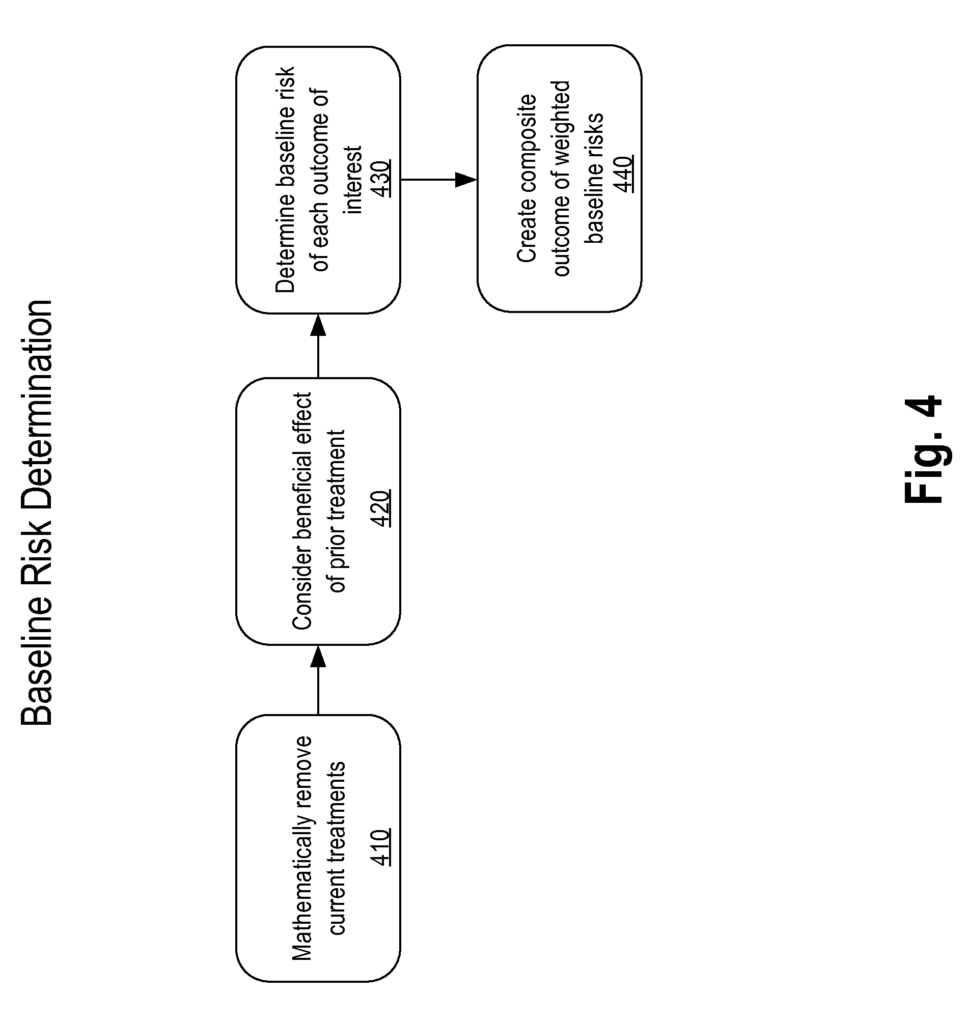
In one embodiment, data representing at least a part of the population’s biomarkers is received. The baseline risk value represents a population’s risk of experiencing one or more health outcomes. The target risk value represents the desired risk that the population will experience the one or multiple healthcare outcomes. A current risk value is also determined, which represents the present risk that the population faces in achieving the one or multiple healthcare outcomes. The potential risk reduction is calculated as the difference between the baseline and target risk values. The current risk reduction is calculated as the second difference between baseline risk and current risk. The current risk reduction value, and at least partially the potential risk value are used to determine a quality score. Assigning the baseline risk and target risk on a scale of quality of care, the quality score is then mapped onto the scale.
In one embodiment, the Archimedes Model is used to receive population data. Archimedes, Inc., San Francisco, Calif., offers the Archimedes model as a commercial service. It is a realistic simulation that has been validated and represents human physiology, disease, and healthcare systems. The Model’s characteristics allow it to support decision-making and research about healthcare systems at a detail level previously unattainable.
In one embodiment, determining the quality score value consists of dividing the existing risk reduction by the potential reduction in risk.
In another embodiment, the assignment of the baseline health outcomes metric and target health outcomes metric on a scale of quality of health care includes assigning a baseline health outcomes metric at a low level of the scale of quality of health care and assigning a target health results metric at a high level of the scale of quality of health care.
In one embodiment, determining baseline health outcomes metrics comprises determining individual baseline health outcomes metrics of each individual in the population, determining sums of individual baselines health outcome metrics of all individuals, and then determining baseline health outcomes metrics. In one embodiment, the baseline outcome metric is calculated per person.
Click here to view the patent on Google Patents.